Managing Trigger Finger: Understanding the Link with Diabetes and Rheumatoid Arthritis

The human hand stands as one of the most intricate structures within the human body, uniquely crafted for tasks ranging from grasping and lifting heavy objects to delicately manipulating small items, such as threading a fine string through a tiny needle eye. Comprising the wrist, palm, and fingers, each hand consists of 27 small joints, an equal number of bones, and an extensive network of muscles, tendons, and ligaments.
However, this complexity can also lead to complex tendon problems like Trigger Finger.
What is Trigger Finger?
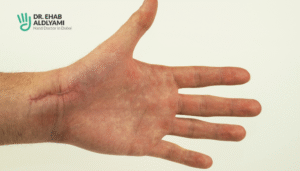
A Trigger finger manifests as a finger that becomes stuck in a bent position, requiring additional effort to straighten it beyond a certain point. Typically, a sensation of clicking or popping is felt at the base of the finger when attempting to extend it beyond this trigger point. While initial triggering may not cause discomfort, over time, it can progress to cause pain and stiffness, inhibiting full finger extension. Symptoms of triggering commonly affect the index, middle, or ring finger, although the condition can also manifest in the thumb or pinky finger.
Triggering arises from inflammation within the finger’s flexor tendon and pulley system, akin to encountering a knot in shoelaces. With each attempt to pass the enlarged tendon through the inflamed pulley, the inflammation exacerbates, perpetuating the triggering sensation.
But does it have any link with Diabetes and Rheumatoid Arthritis?
Trigger finger involves issues with tendons, while arthritis primarily affects joint cartilage; however, these conditions can overlap. Rheumatoid arthritis, for instance, may correlate with trigger finger development.
On the other hand, research studies indicate that diabetes can also indirectly contribute to trigger finger and thumb occurrences.
How can Rheumatoid Arthritis cause Trigger Finger?
Rheumatoid arthritis (RA) is an autoimmune disease characterized by chronic inflammation of the joints, which can lead to joint damage, pain, and stiffness. While RA primarily affects the joints, it can also impact the tendons and surrounding structures, leading to complications such as trigger finger.
However, it’s important to note that while rheumatoid arthritis is a significant risk factor for trigger finger, not all individuals with RA will develop this complication. Early diagnosis and treatment of trigger finger in individuals with RA can help alleviate symptoms and prevent further complications.
Is trigger finger osteoarthritis or rheumatoid arthritis?
Trigger finger can occur in individuals with either osteoarthritis or rheumatoid arthritis, although the mechanisms underlying its development may differ between the two conditions.
In osteoarthritis, trigger finger is typically the result of wear and tear on the joints and tendons due to degenerative changes associated with ageing or repetitive use. As osteoarthritis progresses, the joint cartilage deteriorates, leading to inflammation, bony growths (osteophytes), and changes in the shape of the joint. These changes can affect the surrounding tendons, causing them to become inflamed or thickened and resulting in trigger finger.
On the other hand, in rheumatoid arthritis (RA), trigger finger may occur as a complication of chronic inflammation affecting the joints, tendons, and surrounding structures. In RA, the immune system mistakenly attacks healthy tissues, leading to synovitis (inflammation of the synovial lining of the joints) and damage to the cartilage and bone. This inflammation can extend to the tendons, causing them to become thickened, inflamed, or develop nodules, which can contribute to the development of trigger finger.
While trigger finger can be associated with both osteoarthritis and rheumatoid arthritis, it is more commonly seen in individuals with RA due to the systemic nature of the disease and its propensity to affect multiple joints and tissues throughout the body. However, it’s important to note that trigger finger can occur independently of arthritis, and various other factors, such as repetitive hand movements, trauma, diabetes, or certain medications, can also contribute to its development.
Rheumatoid Arthritis Trigger Finger Treatment
Treatment for trigger finger associated with rheumatoid arthritis typically entails a combination of conservative measures and medical interventions. Conservative treatments may include rest, splinting, and exercises to improve finger mobility. Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections may be prescribed to reduce inflammation and eliminate symptoms.
In severe cases or when conservative lines of treatment fail, surgical options such as tendon release surgery may be considered to relieve tendon constriction and restore finger function. A comprehensive treatment approach, personalized for the individual’s needs and disease severity, is essential in managing trigger finger in the context of rheumatoid arthritis.
How can diabetes lead to trigger finger?
Trigger finger can also be associated with diabetes, although the exact mechanism is yet to be understood fully. In many individuals with diabetes, high blood sugar levels can lead to changes in the structure and function of tissues, including the tendons in the fingers. This can result in thickening or inflammation of the tendons, making them more prone to catching or getting stuck in a bent position.
Additionally, diabetes-related complications such as neuropathy (nerve damage) may contribute to altered sensation and impaired hand function, increasing the risk of developing trigger finger. Proper management of diabetes, including blood sugar control and regular monitoring, may help reduce the risk of developing trigger finger in individuals with diabetes.
How can diabetes lead to trigger finger?
Trigger finger can also be associated with diabetes, although the exact mechanism is yet to be understood fully. In many individuals with diabetes, high blood sugar levels can lead to changes in the structure and function of tissues, including the tendons in the fingers. This can result in thickening or inflammation of the tendons, making them more prone to catching or getting stuck in a bent position.
Additionally, diabetes-related complications such as neuropathy (nerve damage) may contribute to altered sensation and impaired hand function, increasing the risk of developing trigger finger. Proper management of diabetes, including blood sugar control and regular monitoring, may help reduce the risk of developing trigger finger in individuals with diabetes.
Diabetes Trigger Finger Treatment
Treatment for trigger finger in individuals with diabetes typically involves a blend of conservative measures and medical interventions. Conservative treatments may include rest, splinting, and exercises to improve finger mobility. Moreover, maintaining optimal blood sugar levels through diet, exercise, and medication management is crucial in managing the condition of trigger finger.
In some cases, doctors may recommend corticosteroid injections to reduce inflammation and get rid of symptoms. However, if conservative measures do not provide the expected relief, surgical options such as tendon release surgery may be considered to restore finger function. A multidisciplinary approach involving coordination between diabetes management and hand care specialists is essential in effectively managing trigger finger in individuals with diabetes.
Suffering from Trigger Finger symptoms? Consult our hand specialist Dr Ehab Bassim Aldlyami
If you’re experiencing symptoms of trigger finger, don’t hesitate to seek expert care. Our skilled hand specialist, Dr Ehab Bassim Aldlyami, has 25 years of extensive experience and offers comprehensive evaluation and personalized treatments for various hand complications.
Take proactive steps towards relieving discomfort and restoring optimal hand function by scheduling your consultation today.
What is the connection between diabetes and trigger finger?
Diabetes can contribute to trigger finger due to changes in the structure and function of tissues, including the tendons in the fingers. High blood sugar levels can lead to tendon thickening or inflammation, making them more prone to catching or getting stuck in a bent position. Additionally, diabetes-related complications such as neuropathy may contribute to impaired hand function, increasing the risk of trigger finger development.
Does trigger finger have anything to do with rheumatoid arthritis?
Yes, trigger finger can be associated with rheumatoid arthritis (RA). RA is an autoimmune disease which occurs due to chronic inflammation of the joints, tendons, and surrounding structures. Inflammation in RA can affect the flexor tendons in the fingers, leading to swelling, thickening, or formation of nodules, which may contribute to trigger finger development.
What is the medical management of trigger finger?
The medical management of trigger finger typically involves conservative measures and, if necessary, medical interventions. Conservative treatments may include rest, splinting, and exercises to improve finger mobility. Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections may be prescribed to manage inflammation and symptoms. In acute cases, surgical interventions such as tendon release surgery may be considered to relieve tendon constriction and restore finger function.
Can trigger finger be caused by autoimmune disease?
Yes, trigger finger can be caused by autoimmune diseases such as rheumatoid arthritis, wherein the immune system starts destroying the healthy tissues, causing inflammation and tendon damage to the joints and surrounding structures; thus, contributing to trigger finger development.

Related Post

Causes of Hand Pain: From Overuse to Nerve Compression
Your hands are involved in almost everything you do, typing, lifting, cooking, driving, scrolling. So

Does Dupuytren’s Contracture Get Worse Over Time
Dupuytren’s Contracture is a slowly progressing condition that affects the hand, the connective tissue just
What Does It Feel Like When Your Scaphoid Is Broken
From Mild Ache to Lasting Pain – What a Scaphoid Break Really Feels Like! Wrist

Thumb CMC Joint Replacement: A Life-Changing Surgical Option
It would be hard to name an activity in daily life that is not affected

مدة علاج العظم الزورقي: كل ما تحتاج معرفته عن علاج كسر العظم الزورقي
العظم الزورقي هو أحد العظام الصغيرة الموجودة في اليد التي تقع في المعصم. بالرغم من

5 Simple Ways to Prevent Carpal Tunnel Syndrome
Small Changes, Big Relief: Prevent Carpal Tunnel Before It Starts! Experiencing tingling, numbness, or pain